GlobalBioSens
DDIs under climate stress
Have you ever thought about climate change and pharmacological vulnerability?
I do, because I react with massive DDIs myself ...
Climate change, environmental pollution, pharmacokinetics, genetics, receptor activation and DDIs (drug-drug interactions)
The increase in weather extremes, rising air pollution and environmental stress is also changing the physiological conditions under which medicines work. People with a genetic predisposition react differently, earlier and more intensively - often with increased DDIs, pseudo-allergic reactions and toxic accumulation that are not recorded by conventional measurements.
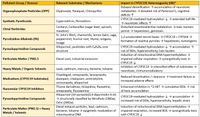
Example synergy: ketoconazole + simvastatin + PM2.5 + ozone + EBV reactivation
Combination effect
- Double AHR activation → ↑ immunomodulation, ↑ inflammation
- P-gp inhibition + CYP3A4 inhibition → ↓ clearance → ↑ tissue concentration
- PM2. 5 + ozone → ↑ oxidative stress, ↑ receptor activation → ↑ pseudoallergic reaction
- EBV reactivation → ↑ cytokine release → ↑ receptor sensitivity → ↑ migraine, brain fog
- possible C/Cb distortion → toxic accumulation in the CNS despite normal plasma concentration
Environmental factors as pharmacological co-drivers i.e. environmental stressors as further (possible) pharmacological modulators
- Metabolism (CYPs, UGTs, NATs)
- Transport (P-gp, OATPs, SLCs)
- Receptor binding (e.g. AHR, TRPA1, HTR2A, ADORA2A)
- Immune response (mast cells, T cells, cytokines)
- Distribution (C/Cb distortion, tissue concentration)
In the future, classical pharmacology should also be expanded to include climate medicine, environmental toxicology and systems biology.
Reflection room PBPK models and GIS
- Would the combination of PBPK models and GIS allow a new form of risk assessment, i.e. individual, spatial and systemic? Could GIS spatially capture and visualize these complex relationships?
- Climate data layers: temperature, UV, humidity, air pollution
- Genetic prevalence layers: CYPs, HLA types, transporters
- Environmental substance layers: VOCs, mycotoxins, pesticides
- Receptor load maps: e. g. AHR, HTR2A, ADORA2A
- Clinical reaction data: Side effects, pseudoallergic reactions
2. Where do climatic stress, molecular triggers and genetic vulnerability meet?
3. C/Cb distortion under climatic stress? Can the concentration of an active substance in plasma (C) under extreme climatic conditions still be representative of the actual exposure in tissue (Cb)?
- ↓ Hematocrit due to dehydration → ↑ C/Cb ratio → Clearance is overestimated
- ↑ Albumin binding during stress → Lipophilic substances “trapped” in plasma → Local overconcentration
- ↑ Distribution in erythrocytes (KpRBC) with lipophilic substances → ↑ Cb → CNS toxicity, immune stress
Standard values such as C or CL may no longer be reliable under climatic stress? Do the current PBPK models already take these distortions sufficiently into account?
4. What about genetic predispositions and metabolic weaknesses? Certain genetic variants influence the ability to metabolize and detoxify drugs and environmental substances:
- CYP3A4↑ Phase I metabolization ↑ Clearance of lipophilic substances, but also ↑ Toxic metabolites
- NAT2↓↓ Acetylation ↓ Detoxification of aromatic amines (e.g. parabens) Parabens, pesticides)
- UGT↓ Glucuronidation ↓ Excretion of mycotoxins, PEG, gallates
- COMT-Val158Met Catechol degradation ↑ Stress response to air pressure drop, ↑ Sensitivity to AHR activation
- HLA-DRB107: 01* Immune presentation ↑ T-cell activation to VOCs, mycotoxins, pollen proteins
- TRPV1/TRPA1 sensory ↑ Perception of temperature, VOCs, pressure change
These genetic factors presumably lead to distorted pharmacokinetics, increased receptor binding and systemic overreaction to climate-related environmental stress.
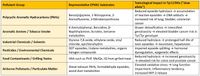
5. Have you already sufficiently considered the increasing drought and low water levels, i.e. possible effects on environmental toxicology and pharmacokinetics?
- Low water levels also lead to the exposure of sediments containing pesticides, heavy metals, VOCs and pharmaceutical residues.
- Drought favors dust formation → ↑ Inhalation of toxic particles (e.g. PM10 with adsorbed xenobiotics)
- Oxidation through UV and air contact → ↑ Reactivity of organic pollutants (e.g. conversion of nitrate to NOx)
These substances are increasingly released into the air, the food chain and drinking water and thus act as an additional burden on detoxification organs.
Possible concentration effects due to water loss
- Less dilution → ↑ Concentration of pollutants in surface waters
Increasing pollution due to:
- Pesticides (e.g. atrazine, glyphosate)
- Pharmaceutical residues (e.g. antibiotics, hormones)
- Industrial chemicals (e.g. bisphenol A, parabens)
These substances can inhibit or activate CYPs, stimulate receptors and block transporters (P-gp, OATPs)
6. Are all climate-related physiological changes sufficiently taken into account?
Extreme climatic conditions such as heat, humidity, UV radiation and air pollution influence key physiological parameters that have a direct impact on pharmacokinetics and pharmacodynamics
Heat
Vasodilation → altered distribution of lipophilic substances
Dehydration → ↓ Plasma volume → ↑ Concentration of lipophilic substances in plasma
↑ Skin permeability → ↑ Transdermal absorption of environmental substances and medications
↑ CYP3A4 activity (temperature-dependent) → altered clearance
Humidity
↑ Mould formation → ↑ Mycotoxin contamination → ↑ Mast cell activation
↑ VOC outgassing from materials → ↑ Respiratory exposure
UV radiation
↑ AHR activation through photoreactive substances → ↑ Immunomodulation
↑ Oxidative stress response → ↑ Receptor binding (HTR2A, ADORA2A)
Air pollution (PM2.5, NOx, O₃)
↑ Inflammation markers (IL-6, TNF-α) → ↑ Immune stress
↑ Permeability of the blood-brain barrier → ↑ CNS toxicity of lipophilic substances
The energy fields and chemical reactions triggered by thunderstorms and lightning may also have indirect but relevant effects on pharmacokinetics. Just a few mind games ...
Pharmacokinetic process Lightning/thunderstorm-related influence
Electric fields and plasma discharges
Lightning is caused by extreme electrical voltages in thunderclouds, i.e. often over 100 million volts. This creates electromagnetic pulses (EMP), which briefly generate strong electric and magnetic fields.
Possible physiological effects
- Neuroelectrical stimulation: High-frequency fields can influence neuronal activity - e.g. by modulating voltage-controlled ion channels.
- Cardiac arrhythmia: In close proximity to the impact, electric fields can disrupt the cardiac excitation conduction system.
- Melatonin suppression: Electromagnetic fields can affect the pineal gland and disrupt the circadian rhythm.
Atmospheric ionization and air chemistry
- Ozone formation: Lightning generates locally high O₃ concentrations → ↑ Respiratory tract irritation
- Nitrogen oxides (NOx): Plasma discharge generates NO and NO₂ → ↑ nitrosative stress, ↑ peroxynitrite formation
- Radical formation: OH- and NO- are formed → ↑ Oxidative stress of the respiratory tract and skin
Environmental toxicological aspects
- Release of soil substances: Lightning can mobilize organic substances in the soil through heat and pressure, e.g. heavy metals, pesticide residues
- Forest fire risk: lightning strikes are a major cause of natural fires → ↑ particulate matter, ↑ VOCs, ↑ mycotoxins due to secondary mold growth
More lightning also means more electromagnetic pollution, more NOx emissions and more fire risks. Perhaps their role in climate medicine, neurophysiology and environmental toxicology is still underestimated and should be given greater consideration in interdisciplinary models?
- Absorption - ↑ Skin permeability through ionized air (plasma effects) → ↑ Transdermal absorption ↑ Respiratory permeability through O₃ and NOx → ↑ Pulmonary absorption of gaseous substances
- Distribution - ↑ vasodilation due to NOx → altered distribution of lipophilic substances ↑ permeability of the blood-brain barrier due to oxidative stress → ↑ CNS distribution
- Metabolism - ↑ CYP activity due to oxidative stress (e. g. B. CYP1A2, CYP3A4) ↓ phase II enzymes (UGT, SULT) due to nitrosative stress → ↓ conjugation, ↑ toxic metabolites
- Elimination - ↑ renal burden due to NOx-induced endothelial stress → ↓ glomerular filtration ↑ hepatic clearance with increased CYP activity, but ↓ with enzyme inhibition by environmental substances
Possible molecular mechanisms
- NOx and O₃ from flash discharges act as radical formers that modulate the expression of detoxification enzymes.
- Peroxynitrite formation (ONOO-) by NOx → oxidizes proteins, lipids and DNA → influences transporters such as OATP, P-gp, MRP2
- AHR activation by photochemically generated substances → ↑ Expression of CYP1A1, CYP1B1 → Altered metabolization of xenobiotics
Exemplary substances with increased sensitivity
- Lipophilic drugs: Diazepam, fentanyl, propofol → ↑ CNS distribution with increased BBB permeability
- Respiratory active substances: salbutamol, fluticasone → ↑ pulmonary uptake in O₃-induced bronchodilation
- CYP3A4 substrates: midazolam, simvastatin → ↑ clearance or toxic metabolites with enzyme induction
Increased thunderstorms and more frequent and intense lightning do not influence pharmacokinetics directly via the drug, but via the body's physiological response to electromagnetic and chemical stimuli. These responses modulate absorption, distribution, metabolization and elimination and could lead to possible altered drug levels, side effects or toxic synergies.
GIS (geo-information systems) and EO data (earth observation, i.e. remote sensing data) could play a decisive role in the field of pharmacokinetics and drug-drug interactions (DDIs) if they are used in an interdisciplinary and forward-looking manner.
Environmental monitoring as a pharmacokinetic context
GIS and EO provide spatiotemporal data on: Temperature, humidity, UV intensity, low water, drought, pollution, land use, pesticide use and industrial emissions
These environmental factors influence: Enzyme activity (e.g. CYPs through AHR activation), transporter expression (e.g. P-gp through toxic exposure) and distribution volume and clearance e.g. through dehydration
GIS could localize and quantify these factors, EO could monitor and predict them.
A possible further DDI risk assessment in the spatial context, because DDIs (side effects) often depend on enzyme and transporter activity.
- Environmental factors modulate these systems → regional differences in DDI risks
- Example: Rifampicin-induced P-gp expression can be enhanced or attenuated by environmental stress
GIS can identify hotspots for increased DDI risks - for example in regions with high levels of pollution or extreme heat
Integration into PBPK models
PBPK (physiologically based pharmacokinetics) uses parameters such as: Organ volume, blood flow and enzyme activity and EO data here could perhaps provide climatic modulators of these parameters. GIS could then link patient location, environmental exposure and medication data, all with the aim of achieving individualized dose adjustment based on environmental profiles.
A possible hypothetical example application: Simvastatin in heat regions
- EO shows: Region X has ↑ UV, ↑ drought, ↑ pesticide exposure
- GIS shows: ↑ myopathy cases with simvastatin in this region
- Hypothesis: ↑ CYP3A4 induction + ↓ phase II detoxification → ↑ toxic metabolites
- Decision: Dose adjustment or switch
GIS and EO data are not classical pharmacological tools, but they are becoming crucial context generators for the safe and effective use of medicines under extreme climatic conditions. They enable a spatio-temporal risk assessment that extends and refines classical DDI models.
CYP2C19 and EPHX1 (epoxide hydrolase 1) also play a crucial role in the metabolization of epoxide-containing drugs and their activity can be influenced by genetic variants, environmental factors and DDIs. This is highly relevant as these enzymes are sensitive to environmental stress, pollutants and climate-induced modulators, which we could capture with GIS and EO data.
Environmental factors such as pesticides, VOCs and AHR-active substances can induce or inhibit CYP2C19, which can lead to DDIs and toxic synergies.
Environmental pollution by epoxide-containing VOCs, e.g. industrial emissions, low water levels, can overload the EPHX1 capacity, which can increase the toxicity of drugs with epoxide-containing metabolites. EPHX1 is a phase I enzyme that detoxifies epoxide-containing intermediates and acts, for example, on cyclophosphamide, carbamazepine, phenytoin, but also on environmental substances such as styrene epoxide, benzo[a]pyrene epoxide. Genetic variants such as Tyr113His, His139Arg influence: Hydrolase activity → ↑ or ↓ epoxide degradation and also the increasing risk of toxic accumulation, DNA damage and neurotoxic effects.
Relevance for GIS and EO data
GIS and EO could here
- Map regional exposure to epoxy-containing pollutants (e.g. styrene, benzene, pesticides)
- Record UV intensity and ozone values → ↑ Epoxide formation through photochemistry
- Localize low water levels → ↑ Release of sediment-bound epoxides
- Spatially represent populations with CYP2C19 polymorphisms (e.g. via genome databases)
This creates a spatio-temporal risk model that shows: Where and for whom epoxy-containing drugs could have a toxic effect under environmental stress conditions. GIS and EO data may enable a very valuable spatio-temporal risk assessment that extends classical pharmacokinetics to include a systemic environmental component.
An Essential Approach for Critical Professions
Firefighters, military personnel, Emergency and disaster manager, paramedics, and other professionals in safety-critical fields face constant health risks, from chemical exposure to infections. A data-driven and preventive health approach is indispensable for their protection. Innovative health strategies should not be missing from emergency planning - they are an integral part of forward-looking security and crisis management concepts. Forward-looking emergency concepts must also take into account ME/CFS, long COVID, loss of smell, medication & drug abuse and polypharmacy.
This contribution was written by Birgit Bortoluzzi, the creative founder of the “University of Hope” – an independent knowledge platform dedicated to resilience, education, and compassion in a complex world. (15.08.2025)